If you’ve ever felt like you have trauma* from having untreated OCD, you’re not alone. That’s certainly how I felt before I did exposure and response prevention (ERP) therapy, the gold-standard treatment for OCD.
OCD causes tremendous suffering. However, sometimes it’s not only the scary content the disorder throws at you that’s the problem. How the disorder treats you and how challenging it can be to get the right treatment can create additional layers of suffering.
In this post, I share an example from my own life of how the experience of OCD can be traumatic. I then discuss several reasons why OCD can feel like a trauma, and offer several ideas for how you can fight back as part of your own OCD recovery journey.
*For clarity, in this article “trauma” refers to an extremely disturbing or upsetting experience, as opposed to post-traumatic stress disorder, or PTSD. A diagnosis of PTSD, according to the DSM-5, requires “exposure to actual or threatened death, serious injury, or sexual violence” as well as meeting other criteria. It’s possible to have both OCD and PTSD, but if you feel traumatized by OCD, that doesn’t mean you also have PTSD.
OCD as a trauma: being held hostage at gunpoint
When I was a teenager, I didn’t yet know I had OCD. What I did know was that I had a mind that could be an abusive tyrant, especially if I threatened to break OCD’s Rule #1 … which is exactly what happened in the following excerpt from Is Fred in the Refrigerator? Taming OCD and Reclaiming My Life about my very first psychiatrist appointment at age 16:
As I sat on Dr. Prasad’s couch, I could feel my mind stirring. I could tell it was angry. I heard it utter swear words as it readied its most deadly equipment, the weapon it brandished in emergencies. Then I heard a telltale metallic clicking and felt the cold hard barrel of a pistol pressed into my temple.
 I tensed. My mind was going to hold me hostage again.
I tensed. My mind was going to hold me hostage again.
Fear coursed through my veins, rose like molten lava in my chest. I could taste its hot malevolence at the back of my throat.
Certain that it now had my undivided attention, my mind thrust forward its manifesto—words scribed in a Satanic-like font reminiscent of a heavy-metal album cover—and screamed, READ IT!
I knew the words by heart. I silently recited them in my head:
You cannot get caught doing these things or thinking these thoughts.
Because if you do, you will have to explain yourself.
And you don’t tell what you see in your mind.
Because if you do, all those bad things you see … you will make them happen.
I nodded assent, telegraphing to my mind that I understood. That I would not break Rule #1. Now. Or ever.
My mind relaxed a little, but it kept the gun’s cool, polished barrel kissing my temple. Lest I forget, or let this nice man sweet-talk me into revealing too much.
Untreated OCD can be traumatic
If you live with untreated OCD long enough, you can begin to feel traumatized by the experience of having the disorder. OCD can be a ruthless voice: it yells at you, degrades you, shames you, slams a mental gun into your temple.
It also screams that you’re not good enough so often and so loudly that eventually you can start to believe it.
These abusive tactics are (as odd as this is going to sound) a strategically smart move on OCD’s part. If its taunts make you feel weak and disempowered and unable to do your ERP, then it gets to maintain control of your life, which it desperately wants to do.
But the trauma that is untreated OCD doesn’t stop with its abusiveness, because there are other aspects of the disorder that can be equally traumatizing:
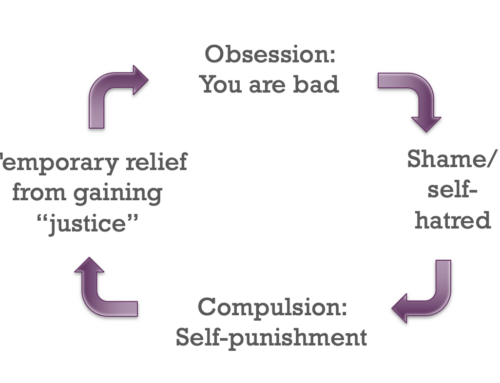
- Shame-inducing obsessions: The frightening content of obsessions, where you think you’re a pedophile, a killer, or a cheater. Or that you’re about to die, eternally burn in hell, or end up locked away in a federal penitentiary. And these are only a small sampling of the types of intrusive thoughts people with OCD experience, all of which make you feel like you’re just bad.

- Exhausting compulsions: The demanding nature of compulsions, where you spend hours and hours doing exhausting physical or mental tasks that you don’t want to be doing, but you can’t seem to stop. And sometimes—if your OCD is as big of a jerk as mine can be—while you’re doing all these compulsions, you feel as though OCD’s mental gun is kissing your temple.
- Additional diagnoses: OCD often has co-conspirators, including depression, other anxiety disorders, body dysmorphic disorder, addictions, body-focused repetitive behaviors, ADD/ADHD, and/or PTSD (and others), all of which can make functioning much harder.
- Stigma: Unfortunately, many people still feel stigma around having any sort of mental illness. Then there’s the additional pain from having a disorder whose name is often thrown around as a joke, as though having OCD—a joy-crushing, debilitating illness (for Pete’s sake!)—is a good thing. Which can make you wonder, “Hey, if everyone’s a little OCD and can talk about it so casually, what is wrong with me that I can’t seem to handle all this?”
- The treatment slog: The often years-long (and sometimes decades-long) slog to find appropriate treatment, which can include feeling misunderstood by loved ones and professionals, being misdiagnosed, and receiving the wrong treatment (sometimes repeatedly), which can all strengthen the OCD and make you feel like you’re somehow “unfixable.”
Moving from victim to survivor
If any of this resonates with you, what can you do? I unfortunately don’t know of any evidence-based answers to this question, but I will share what I have done personally as part of my own OCD recovery and how I help my clients with OCD as a trauma.
Stand up to OCD!
OCD therapists often have kids with OCD talk back to their OCD monsters to help the children feel empowered, and this technique has been one of the most important skills of my own recovery. Except … I don’t just “talk back.” I yell. Loudly. Powerfully. And with my Shoulders Back. It might sound something like this:

OCD, you think you’re gonna keep ruining my life, you [insert favorite swear word combination here]? Well, you got another thing coming, because I’m not letting you call the shots anymore! I’m in charge, I make the decisions. You have made my life a living hell, and it’s payback time. I’m doing exposures, I’m making myself anxious, I’m bringing it on, you [more favorite swearwords here], and I’m going to win. You hear me? You hear what I’m saying? I’m not going to be bullied by you any longer! I’m stronger than you are, and I’m taking my life back. Starting right here, right now, my life is my own. You can yell at me, you can make me anxious, but I’m not doing what you say anymore. I’m going to use everything you throw at me to do exposures, you [final fun swear words 😊] because I am NOT your victim, OCD. I am strong, I am a survivor, and I AM GOING TO WIN!
When I’ve had clients who’ve felt traumatized by their OCD stand up, put their hands on their hips and their Shoulders Back and yell words like this at OCD, it often turns out to be one of the most empowering exercises of their recovery journeys. Many of us with the disorder don’t even know it’s possible to yell at OCD, but it is. You can put OCD in its place. You can claim out loud that you’re not going to stand for the abuse any longer, that things are changing, and that you CAN do this.
If your OCD is yelling at you, what would it be like for you to yell back at it?
Be self-compassionate
Self-compassion is treating yourself like you’d treat a good friend, and it’s the opposite of how OCD treats you. Deploying self-compassion is a great way to fight back against the abuse that OCD can hurl at you. It also builds a strong foundation for your recovery. To learn more, I’ll refer to you Kimberley Quinlan’s book, The Self-Compassion Workbook for OCD: Lean into Your Fear, Manage Difficult Emotions, and Focus On Recovery, and posts I’ve written about the topic, including:
- Aha! Moments from Self-Compassion
- Don’t Talk to Me Like That! Maximize Your Recovery using Self-Compassion
- Power Up Your OCD Recovery Self-Compassion Worksheet
- Show Yourself Some Love!
You do not deserve abuse, from OCD or anyone. If OCD is abusing you, you can try the two step process of 1) giving it a piece of your mind (see above) and 2) being extra kind to yourself, a combination that strengthens you while weakening OCD.
Get professional help
I recommend that everyone with OCD work with a trained ERP therapist if possible, especially if you feel traumatized by your OCD. A therapist can assess your situation, including whether you have a history of trauma or diagnosable PTSD that might make you especially susceptible to feeling traumatized by OCD, and identify any additional treatment approaches that might be beneficial for you—so that you can go from feeling like a traumatized victim to becoming an empowered survivor.
Make your voice heard
 I often wonder if:
I often wonder if:
- Feeling traumatized by OCD can interfere with ERP in a variety of ways, and
- If addressing OCD as a trauma therapeutically could help people who feel stuck in their recovery journeys to move forward more productively.
Share your thoughts
If this article resonates with you, please scroll all the way to the bottom to where it says Leave A Comment and share your thoughts to help all of us better understand and address OCD as a trauma. You can do so anonymously by using initials or a pseudonym if you don’t want to share your name. The email address that’s required is only used by my website to weed out spam, is not displayed publicly, and will not add you to any mailing lists.
Participate in an ongoing research study
And as an exciting update, coincidentally Dr. Caitlin Pinciotti, Assistant Professor in the Menninger Department of Psychiatry and Behavioral Sciences at Baylor College of Medicine, is running a research study right now about OCD and trauma that you can participate in! She hopes that findings from this study will help us finally start to understand how and why OCD and trauma sometimes mix, and how we might be able to better diagnose and treat individuals with these experiences.
Learn more about taming OCD
Sign up for my Shoulders Back! newsletter to receive OCD-taming tips & resources, including notifications of new blog posts, delivered every month to your inbox.
My blogs are not a replacement for therapy, and I encourage all readers who have obsessive compulsive disorder to find a competent ERP therapist. See the IOCDF treatment provider database for a provider near you. And never give up hope, because you can tame OCD and reclaim your life!
Picture credits: Traumatized woman © Can Stock Photo / Tinnakorn; No bullying © Can Stock Photo / rmarmion; Comments box © Can Stock Photo / iqoncept


If this article resonates with you, please share your thoughts, as I’d love to generate enough comments on this post to inspire research studies on this topic.
You can do so anonymously by using initials or a pseudonym if you don’t want to share your name. The email address that’s required is only used by my website to weed out spam, is not displayed publicly, and will not add you to any mailing lists.
I was thrilled to see the title this article. I am a mother to a grown son who has dealt with severe OCD since he was about 5. I’ve spoken to a couple of his therapist about the possibility that he needs treatment for the trauma OCD causes. It seems to me the that the horrible narrative that OCD creates in the mind can have almost the same effect as living with an abusive parent. I feel dealing with OCD through childhood, the years that shape your view of yourself and the rest of the world causes a lot of damage to self-esteem , confidence, and makes it hard to know your own identity. I would love to see this addressed by therapist!Thank you for your insight!
Thank you so much Shala….!
Thanks Shala for shining a light on this. It is important. The challenge I’ve experienced with OCD related trauma is that seeking to avoid it can become an obsession in itself. I did not appreciate it initially – thinking it was my old themes coming back to haunt me. Doing ERP on the wrong themes become a compulsion and only made it worse. What a mind bender! So grateful for a specialised OCD psychologist/therapist who could identify what was happening and help me find my way out.
Very relevant article to anyone who struggles with this debilitating disorder or knows someone who does.
Thank you🙏 This article is motivating — Do not give up, keep going and you are not alone💕
And I just followed Kimberley Sage’s advice “do hard things” Leaving a comment is incredibly hard for me! OCD takes over! BUT I confronted it🥊☺️
I believe that OCD should been treated with a range of tools . I have had OCD for 30+ years and only been treated 2 years ago . Not knowing what was wrong with me , getting wrong treatment and affecting other people have all been traumatic . ERP helps but ongoing treated for trauma and how to live productively without it is so important . It is a recovery journey . I am reading about polyvagal theory which helps PTSD and doing practises that are helping me process trauma . Thank you for highlighting this aspect
I know that challenging ocd is a huge part of being able to deal effectively with it to help in regaining control of your life, but I don’t think we emphasize strongly enough, that what we are being asked to do is a monumental task. To face our fears which are absolutely terrifying and to do it over and over is almost a superhuman endeavour. We need to remember that and realize that if we fall sometimes or feel overwhelmed, we have the right to step back and give ourselves some space for peace and ease. I’m not talking about giving up. I’m saying, you’re human, and be proud of any step you take towards recovery no matter how small.
Shala,
Thanks again for the open forum to share with fellow travelers on this fabulous journey of life through the prism of OCD. I have struggled with anxiety since I was a young boy, starting with memories of going to the doctor for a hearing test and asking for my Marine Corps veteran/firefighter father to pull the car over to the side of the road so his scared little son could throw up. Just the first of many such incidents, no matter what the fear or anxiety provoking experience. By the time I became a teen, the full blown harm OCD began to raise its ugly head. The unknown monster in my head waxed and waned until it finally brought me to my knees at the age of 36. Untreated OCD is truly traumatizing. Long story, short, Meds and talk therapy helped, but as you practice, ERP is the gold standard! I have done most of the work through self study, thanks to dedicated professionals like yourself making great resources available to your fellow sufferers. I am 64 now, and feel I have finally turned the corner to being in recovery. It is a daily battle, but I won’t give up! The one thing I continue to notice, and it may be a sign of the trauma, is a nagging feeling of dread that seems to creep into my mind almost every day and follows me in my most quiet and restful periods, like in the evening when it’s time to relax and enjoy TV time with my spouse. I know it’s just ugly old OCD trying to steal the show, but something I look forward to overcoming in the near term. Your co-authored book is on its way, and I’m confident it will provide some refreshing new tools for winning the war!
All the best,
Alex
How can you help a young adult who believes the trauma they have is from ERP itself, done in an intensive outpatient teen program at one of the best programs in the country? The believe is that it’s better to live with extreme OCD than to do ERP again? BTW I loved your book! You’re an inspiration!
I experienced trauma from decades of untreated OCD and the lowest of lows… I think researching trauma/ocd would be invaluable. Thank you for this article!
I actually wonder if a diagnosis of PTSD COULD be given because the criteria just require the “threat” of death, violence, or injury. And OCD certainly has us believe the threat is real.
Debbie
Thank you Shala for your “Everyday Mindfulness” workbook. emphasizing self-compassion has helped me since experiencing my fifth major episode of ocd, relapsing in January of 2021 after getting covid. This post of yours on OCD and Trauma is very timely for me, as i have often wondered why i’ve never read or heard discussions at conferences about the possibility of the experience of ocd also being considered a trauma –i can tell you it certainly has been one to me after having these 5 major episodes since i was 25 and i’m 69 now. i can tell you the link is now being looked at by researchers and therapists, maybe not with ocd specifically, but with anxiety, depression and even chronic fatigue syndrome. i attended an on-line “Anxiety Super Conference ” and they discuss dysregulation of the nervous system and various therapies/modalities for re-setting it. i also watched an introductory video Called “Why therapy Isn’t Working” by a Dr. Aimee Apigian, a leading medical expert on addressing stored Trauma in the Body. this is an introductory video to her 21 day experiential course. She teaches on various states of the nervous system and has develped a step by step process to be followed before, as she claims, that many forms of therapy can have an effect. she says you first need to develop a sense of safety in the body by creating new experiences and is the only way we can change, because it helps you break out of these old patterns. in just dealing with the mind in therapy, the body and nervous system have not been addressed. She says there is a biology and body component to trauma, and through a combination of guided exercises of somatic (body) work, you will understand your body on a deeper level, and recognize your unique way in which stress and trauma has impacted your body. we need to “re-wire” ourselves! i agree with Penny above, especially when you’ve had ocd a long time, you need many modalities/therapies for recovery. Penny mentioned Poly-vagal theory which i believe are some of the exercises Dr. Aimee uses, and mindfulness is also a way to re-wire our neural pathways. again, it’s not just about healing the mind , but also healing the body, and i think in the future there will be more progress being made in dealing with ocd and the hope for recovery.
This is SPOT ON! Thanks for raising awareness to this really important, and often unacknowledged, topic, Shala! As a psychologist that specializes in treating OCD, we need to see more on this topic. I would love to see a deeper exploration and differentiation between chronic and acute trauma related to OCD diagnosis. By this I am referring to the fact that OCD can have both an insidious onset that unfolds chronically, or an acute and severe onset, to which an individual responds as they would to some other acute trauma (e.g, car accident, near death experience). There are important differences. I’ve had patients who have to deal with the acute trauma of experiencing sudden-onset OCD and not knowing what it was…and then the subsequent trauma of realizing it is OCD, followed by the identity crisis that ensues when one is diagnosed with (and immediately stigmatized by) a mental health diagnosis.
Hello. I am both a therapist and survivor of OCD!! Definitely have symptoms of trauma to this day and believe that most of us suffer untreated OCD. While I continue to do my own work, this should definitely be considered in treatment. Thanks for the article!!
Such an important topic that we must consider when treating clients with OCD. Thank you Shala for another wonderful article
Shala, I am so grateful for your bravery in sharing your experiences. I am learning so much from your newsletters and articles!
I have often wondered the same about OCD causing trauma – it certainly has affected my life in a traumatic way. I do hope that research can be done into this topic to bring insights and hopefully a sense of understanding to those who suffer from OCD.
I second “N” in that typing this comment was also a “do hard things” challenge for me today! Thank you for this opportunity!
I am most interested in the relationship between OCD (and other co-morbids, such as misophonia) and trauma: how the disorder itself, or being neuroatypical, creates complex trauma. You have touched upon it; I would love a dialogue about the other imapcts of complex trauma tjt arises from years of hupervigilance, sensory overload, inherent fear/anxiety in daily living. thank you for your work!
This! This! This! And the world of psychology, for the most part, is utterly ignorant regarding this. CBT, ERP, can be so traumatizing to those who, after years of hyper-vigilance, do not have enough nervous system capacity to withstand the distress of even the smallest exposure. Mine has a panic attack at the thought of talking to yet another therapist. Living with severe OCD is definitely trauma inducing, but OCD can also act as a mechanism to prevent the trauma of loss in those previously traumatized by PTSD/CPTSD. Until that trauma is addressed, OCD treatment of CBT/ERP, the “gold standard”, can actually add to the suffferers trauma. I’ve only found 2 clinicians that get this and neither are in my state. The damage others have done (4 prior therapists) have caused trauma all on it’s own. I literally shake trying to search for someone to help my daughter, who has severe OCD and is on the autism spectrum.
At some point this year I’m hoping to write a blog about what is called post-traumatic OCD, or a merged case of PTSD and OCD, where the OCD acts as an avoidance mechanism to keep the trauma from happening again. I learned about this subtype of OCD in 2019 at the International OCD Foundation conference in a talk led by Nathaniel Van Kirk, PhD. You can read a paper he co-authored about this concept called “Implications of comorbid OCD on PTSD treatment: A case study” at https://pubmed.ncbi.nlm.nih.gov/30589581/ to learn more. But the good news is that post-traumatic OCD can be treated with a combination of evidence-based treatment approaches for OCD (ERP) and PTSD (prolonged exposure and/or cognitive processing therapy). In my work on cases of PTOCD since 2019, I’ve found that for some people starting with the trauma work provides a good foundation to be able to eventually work on the ERP. I hope that helps!
Thank you so much for your willingness to keep learning and help those who suffer from comorbidities and don’t fit immediately into standard treatment protocols but need further consideration. My question is this, if this has been known since 2019 why are there still so few OCD therapist who know nothing of those who suffer most (PTSD+OCD) and are liable to suffer triggering and even more trauma from standard ERP treatment? Please do all you can to help educate fellow therapists in this much needed specialized area. If you can recommend any therapists that get this, have worked successfully with PTSD+OCD and that are licensed in Texas or who (via Psypact) can offer services in Texas, I would be most grateful.
Try the Anxiety and Trauma Clinic of Atlanta https://www.anxietytraumaclinic.com/, as I believe some of their therapists are PSYPACT certified, and I’ve worked jointly with at least one of the therapists there for mutual clients who had OCD and PTSD. I hope that helps!